Designing for Health Equity- Focussed Healthcare Platform
In 2023, I led UX strategy for a two-week design pitch focused on improving how a healthcare platform supports health equity using Social Determinants of Health (SDOH) data. Along with a principal designer and a senior consultant, I helped shape the problem, define what was realistic within the timeline, and deliver a functional prototype that showed how wellness coaches could make better, more informed decisions for their members.
👉 This is a public, NDA-safe overview of the work that shows how I led design decisions through ambiguity in a healthcare environment with strict time and data constraints..

The context
Healthcare platforms today rely heavily on wellness coaches to guide members beyond medical data — helping with lifestyle, access to care, and everyday challenges.
Factors like housing, employment, income, food access, and transportation play a huge role in health outcomes. These are often referred to as Social Determinants of Health (SDOH).
The challenge is that:
- This information is often incomplete or hard to access
- Privacy limits what data can be used
- Coaches still need clear, practical guidance — not raw data
Our goal was to explore how SDOH insights could actually help coaches in their daily work, not just exist as extra information.
organization
Emids
INDUSTRY:
Healthcare
TIMELINE:
March 2023 (2 weeks)
Team Members:
Swati Soni
Sr. Lead Product Designer
Mohd. Asif
Principle Designer
Abhinav Singh
Sr.Manager, Consulting
My role
I led UX strategy and design direction for the project. That included:
- framing the problem we wanted to solve
- guiding early discussions and prioritization
- shaping workflows and system concepts
- making scope decisions within a tight timeline
While we worked as a team, I was responsible for driving clarity and aligning the solution with real-world constraints.
The problem we focussed on
Wellness coaches manage many members at once. Today, it’s hard for them to:
- understand a member’s real-life challenges quickly
- know who needs attention first
- turn insights into clear next steps
Even when SDOH data exists, it’s often:
- scattered across sources
- difficult to keep current
- hard to apply during real conversations
The real problem wasn’t “how do we collect more data?”
It was how do we help coaches make better decisions with the information they already have?
Key constraints
- Timeline: 2 weeks
- Data access: Limited due to privacy and policy constraints
- Audience: Busy wellness coaches, not analysts.
- Goal: A strong, realistic proof of concept – not a production system
These constraints helped us stay focussed instead of over designing.
Our approach
1. Staying grounded in realistic data
Instead of relying on hard-to-access external data, we focused on sources that could realistically exist inside a healthcare platform:
- health risk assessments (HRA)
- employment and insurance context
- insights gathered during coach–member interactions
This kept the solution practical and defensible.
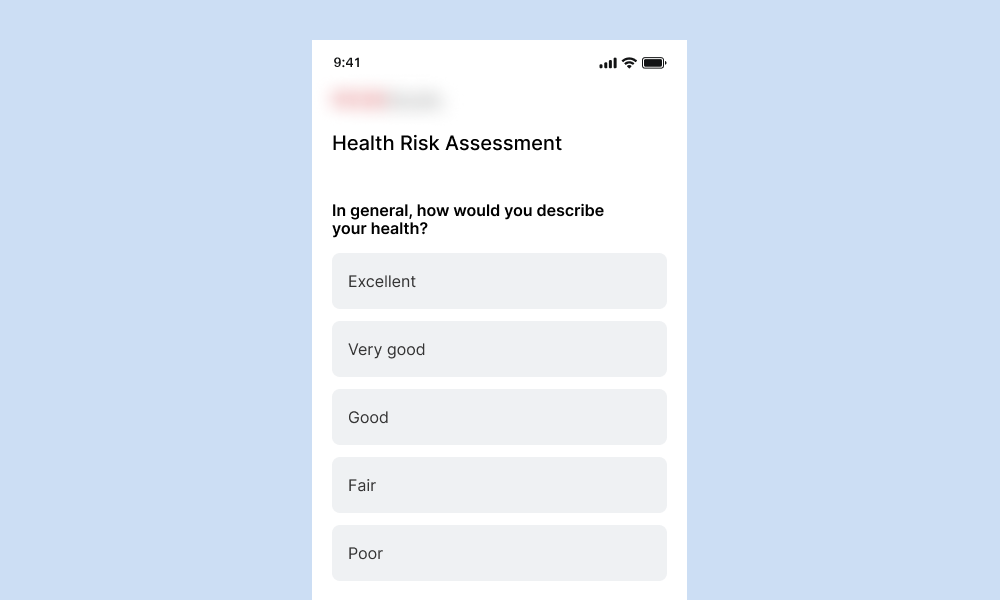
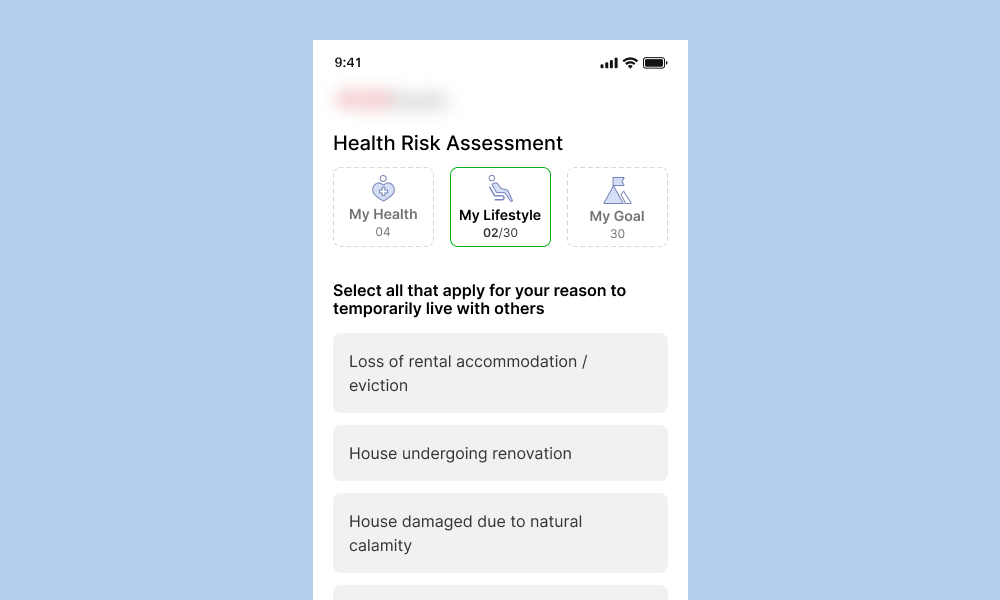
Drag the slider to view enhancements in the survey screen UI.
The HRA survey was updated to include questions on nutrition, housing, income, and expenses, helping us better understand a user’s living conditions. We also used insights from wellness coach interactions and available employment or insurance data to build a more complete picture.
2. Defining a focussed MVP
SDOH is broad. We intentionally limited scope to insights that:
- directly helped coaching decisions
- could be explained clearly in a pitch
- avoided complex or opaque scoring logic
This helped us move fast without losing credibility.
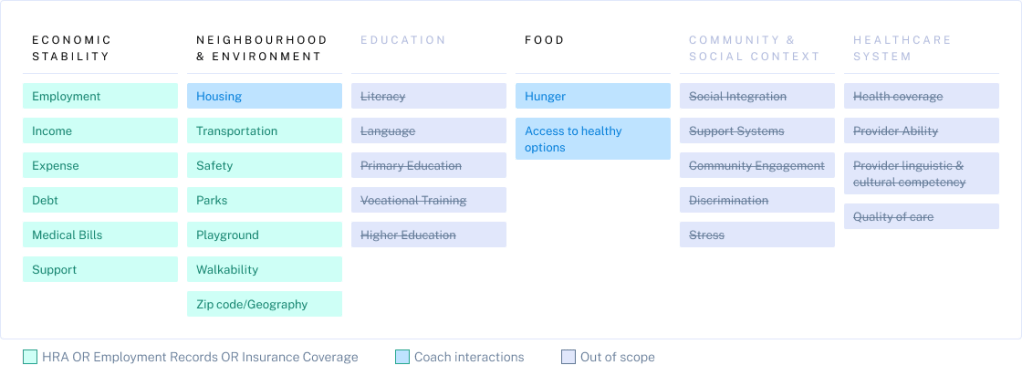
This visual highlights the Social Determinants of Health (SDOH) recognized by the UN.
For the proof of concept, we scoped a subset of these factors—specifically those that were easier to collect and validate—allowing us to demonstrate value quickly while keeping the solution practical.
Key design decisions
1. Helping coaches prioritize at a glance
We introduced a simple Health Equity Score to help coaches quickly see which members might need support.
- It provides a quick signal, not a diagnosis
- Coaches can drill down to see context behind the score
- The goal was speed and clarity, not precision
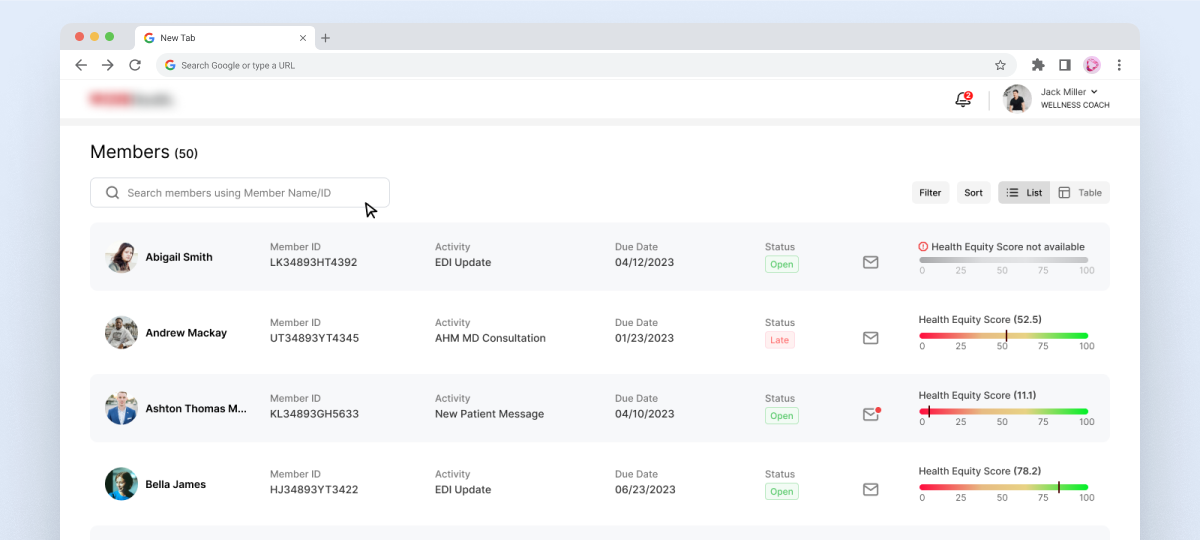
The slider visually indicates the severity level and helps identify how urgently action is needed for each individual.
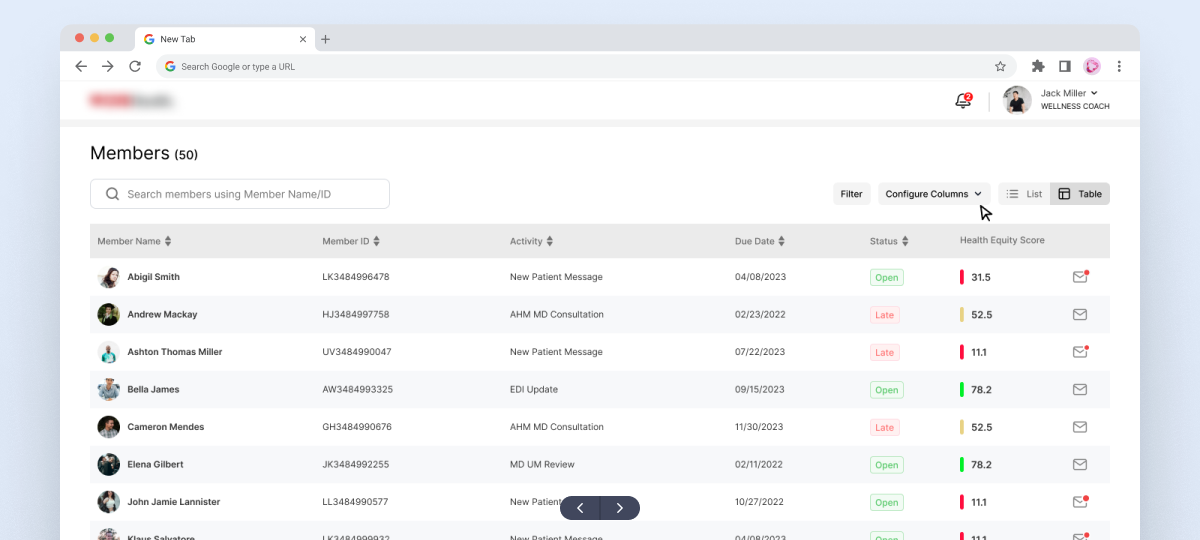
This format allows more data points to be viewed at once. A simple toggle lets wellness coaches switch easily between list and table views, based on how they prefer to review information.
2. Giving coaches a single, clear view
Instead of spreading information across multiple screens, we created a single overview that showed:
- Nutrition and housing context
- Income and expense indicators
- Notes and current action plans
This reduced back-and-forth and helped coaches prepare for conversations more effectively.
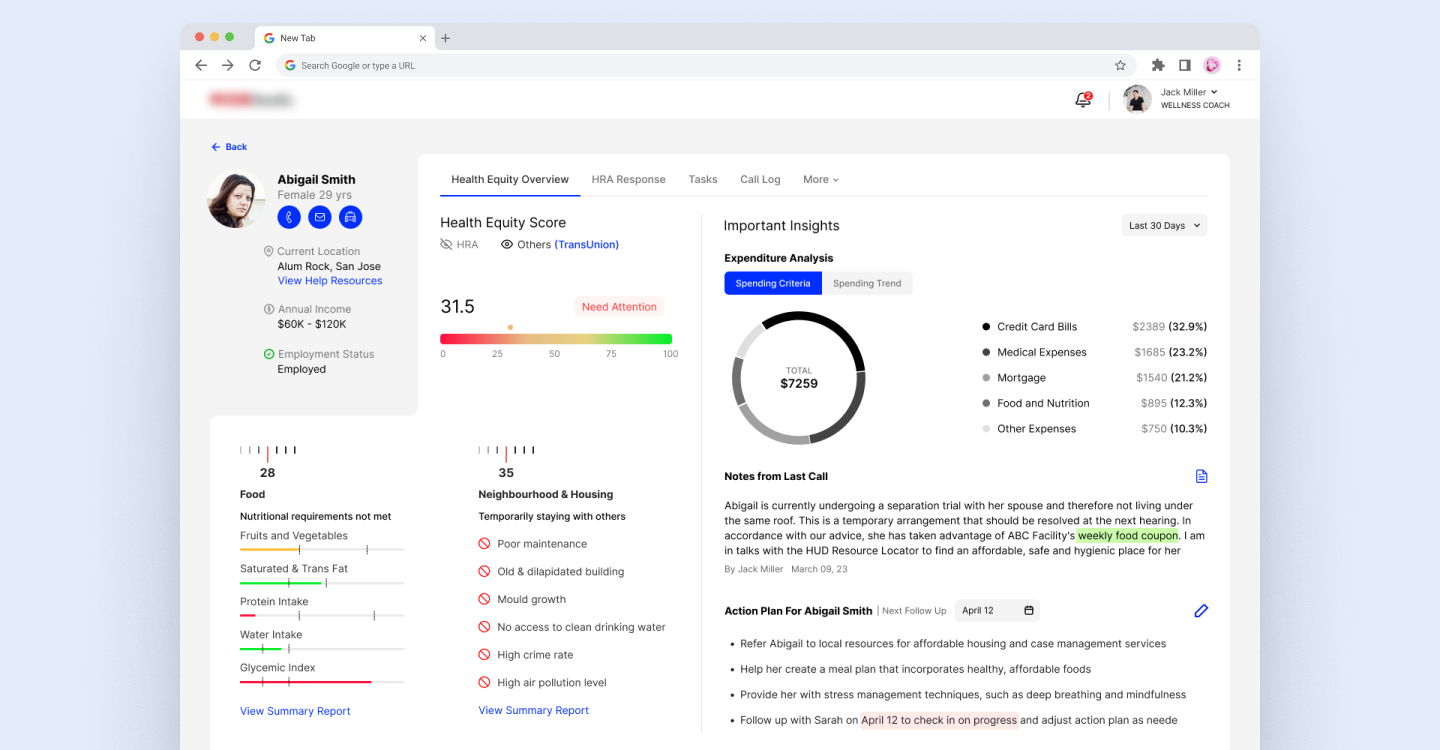
This gives wellness coaches a quick, consolidated view of the user’s social and living conditions without navigating across multiple screens.
3. Making documentation easier
Coaches spend a lot of time documenting conversations. To reduce friction, the concept included:
- AI-assisted summaries from call transcripts
- Structured note-taking for sensitive data
- Visual cues to highlight important concerns
The focus was on supporting coaches, not replacing their judgment.
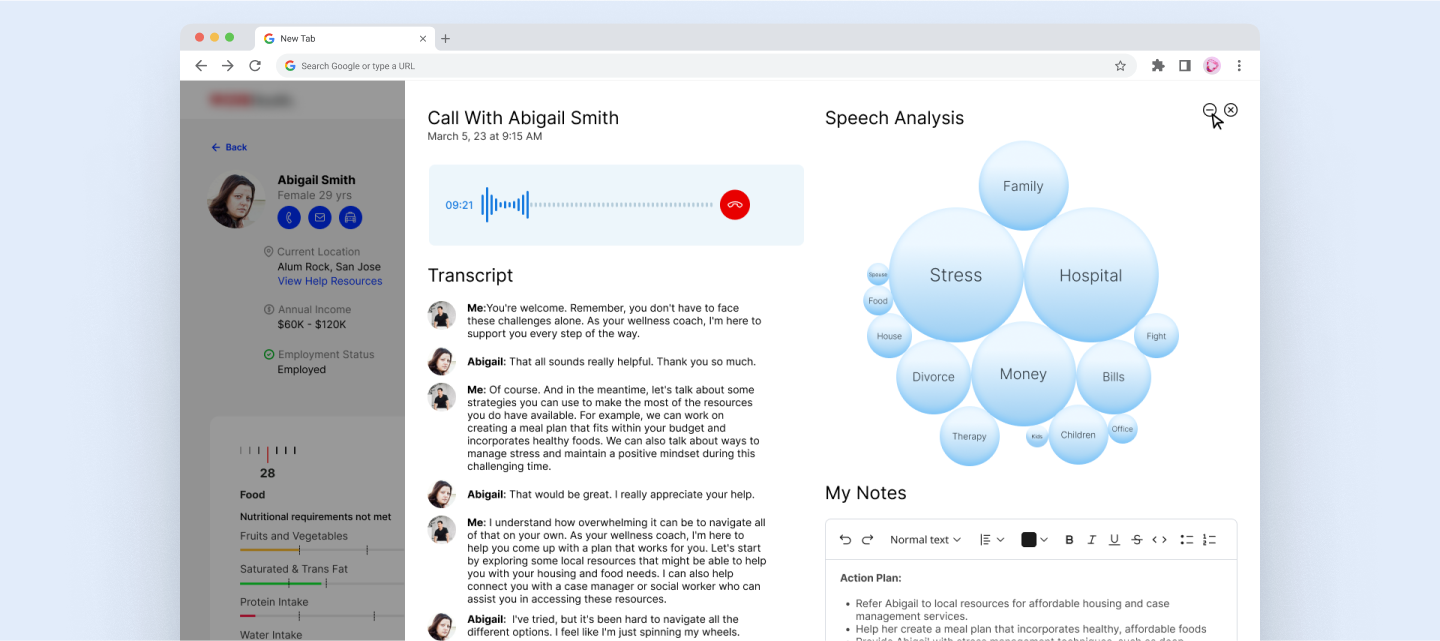
Using third-party speech analysis, the system identifies key themes from the conversation and shows how frequently they were mentioned. This helps coaches better understand the employee’s current state of mind and the key challenges they may be facing.
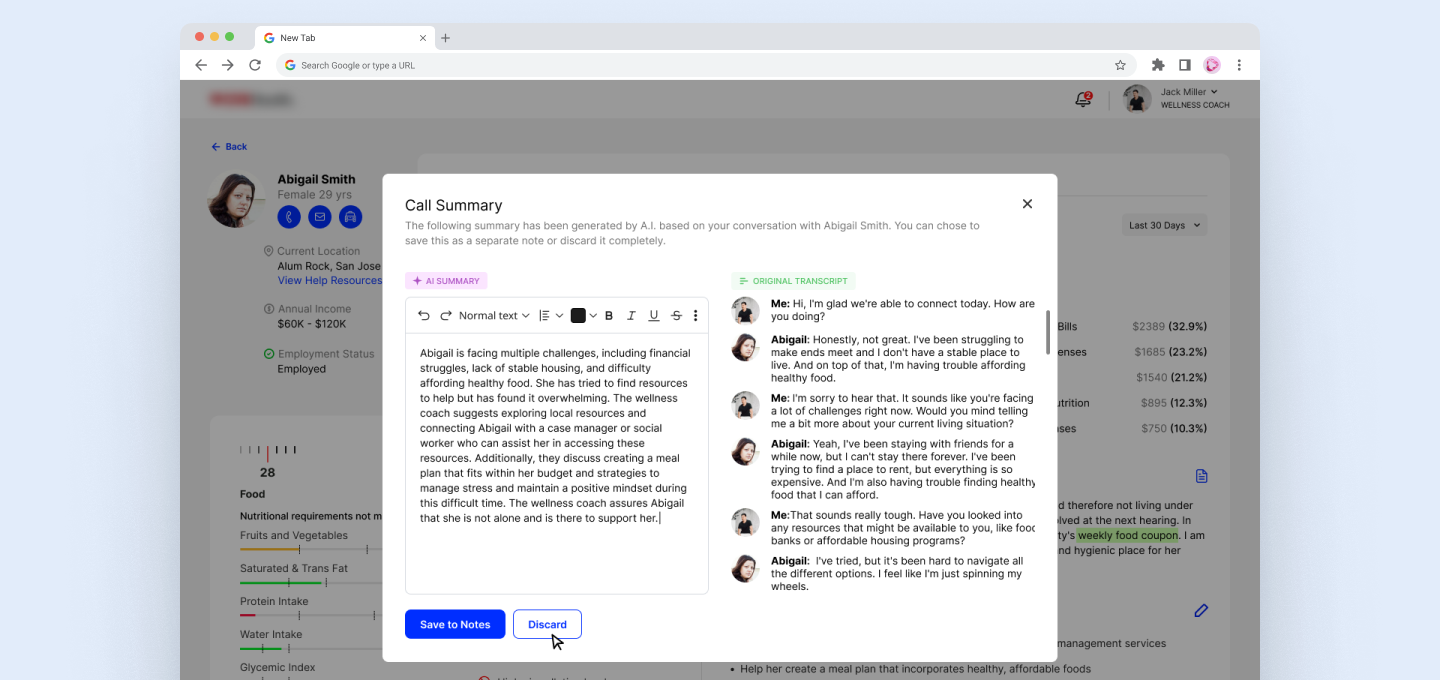
These summaries serve as a starting point, allowing wellness coaches to review, edit, and refine the notes to ensure all key details are accurately captured.
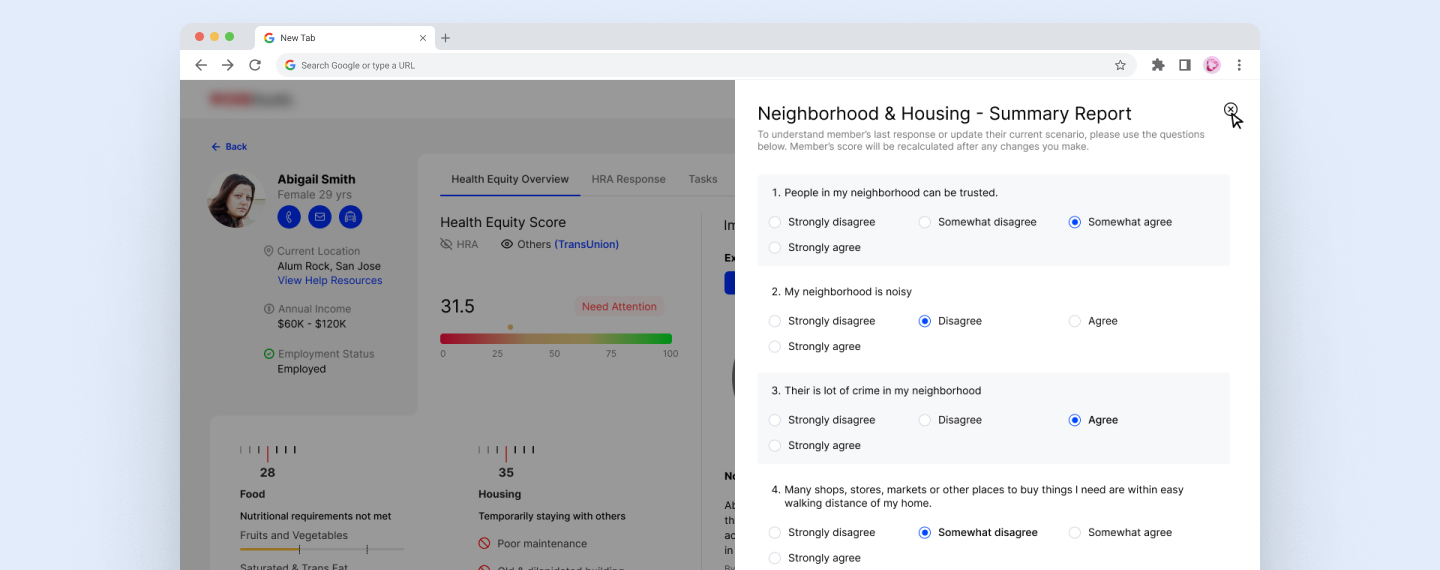
During a 1:1 conversation, wellness coaches can minimize the call recording window and open the survey to capture employee responses in real time. These inputs help determine or update the employee’s Health Equity score.
4. Connecting insights to action
We added a location-based resource search so coaches could quickly find:
- Food banks
- Healthcare services
- Community support programs
This helped turn insights into practical next steps.
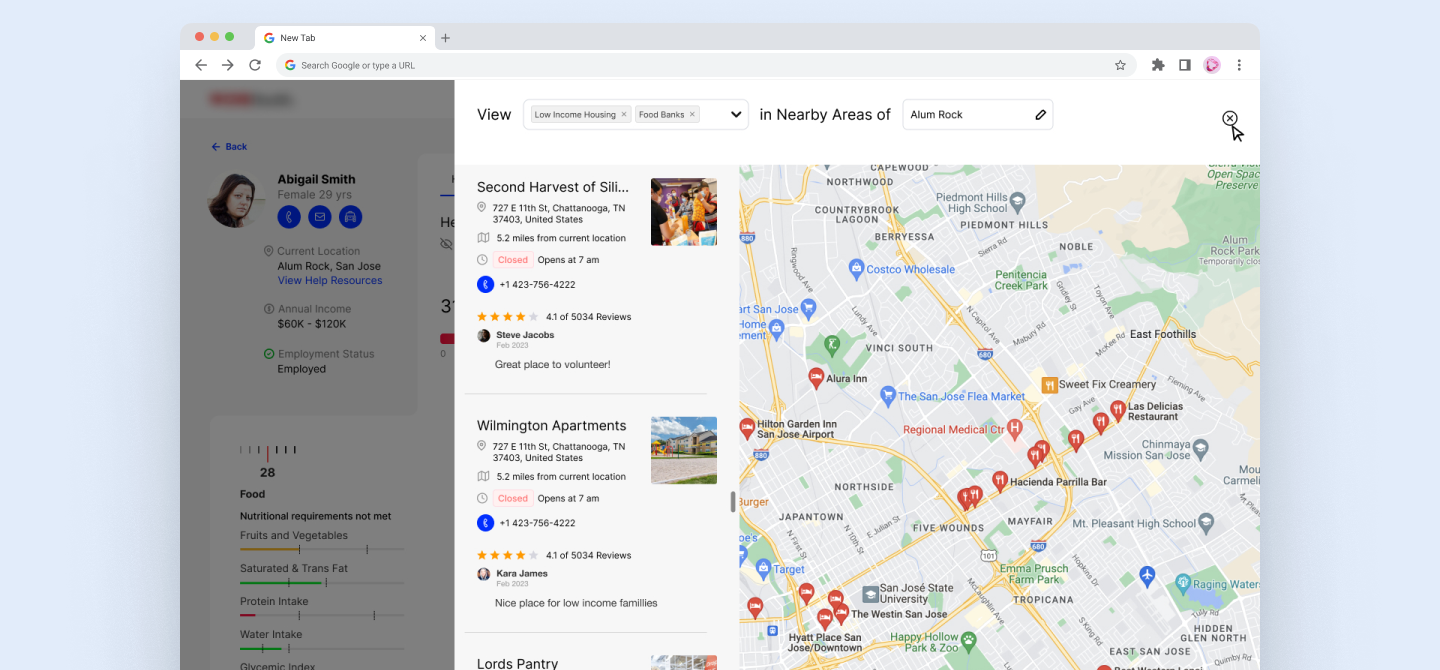
Coaches can view and edit the location to see nearby support options—such as food banks or low-income housing—and guide employees toward relevant local resources, if needed.
Outcomes and learnings
The pitch was received positively and helped demonstrate a clear, thoughtful approach to using SDOH responsibly.
Key learnings from the project:
- Focus matters more than feature count
- Health equity works best as decision support, not raw data dashboards
- Clear scope and prioritization are critical under tight timelines
For me, the exercise reinforced that leading design in complex healthcare spaces is often about making smart trade-offs, not chasing completeness.
Why this work matters
Health equity isn’t solved with more screens or more data.
It’s solved by helping people make better decisions in real situations.
This case study reflects how I approach design leadership:
- Keep things understandable
- Respect real – world constraints
- Design for people making time-sensitive decisions
